Updated on March 25, 2025
Night Blindness Statistics


Vision Center is funded by our readers. We may earn commissions if you purchase something via one of our links.
Night blindness, also known as nyctalopia, affects how people see in dimly lit conditions or after dark. Though not one of the most widespread visual impairments in the United States, it can severely limit mobility, driving, and overall quality of life when it does occur. This article presents a comprehensive, data-driven look at night blindness: how often it occurs, its common causes, and the tangible impacts on individuals and public health.
Night blindness is not a disease in its own right but rather a symptom linked to other eye conditions or deficiencies. In many developing regions, it is frequently caused by poor nutrition (especially vitamin A deficiency).
In the U.S., however, night blindness arises mostly from age-related eye diseases such as cataracts or from inherited retinal disorders like retinitis pigmentosa (RP). Over the past 10 years, overall prevalence in the U.S. has stayed relatively low; nonetheless, with an aging population, the absolute number of Americans reporting some degree of night vision trouble has edged upward. Understanding who is affected, why it happens, and how it can be addressed is essential for reducing road hazards, preventing falls and injuries, and supporting greater independence.
Key Statistics at a Glance
- Night blindness prevalence in the overall U.S. population is relatively low (far below 1%) when purely defined by nutritional deficiency, but increases with age-related eye conditions.
- Retinitis pigmentosa, a major genetic cause of night blindness, affects roughly 1 in 3,500 to 1 in 4,000 Americans, or about 100,000 people nationwide.
- Cataracts, present in over 24 million Americans age 40 and above, are the leading reversible cause of night vision problems, with a treatment success rate exceeding 95% for restoring clearer vision.
- About 20% to 50% of older U.S. drivers limit or avoid driving at night due to vision concerns, reflecting the significant lifestyle impact of poor night vision.
Prevalence and Broader Demographics
Night blindness in the U.S. largely mirrors the broader state of national eye health. This section is key to understanding the overall scale of nyctalopia, including how it compares to other forms of visual impairment.
- General Prevalence:
- Nutritional deficiencies (particularly vitamin A deficiency) account for very few night blindness cases in the U.S., with estimates placing vitamin A deficiency at around 0.3% of the U.S. population in recent years.
- Most reported cases of ongoing or progressive night vision loss instead stem from cataracts, retinal disorders, or other eye diseases.
- Globally, night blindness rates can exceed 1% in regions with poor nutrition, but such high levels are unusual in the United States.
- Age-Related Trends:
- Older adults constitute the largest at-risk group due to cataracts, glaucoma, and other age-related ocular changes. By age 80, more than half of Americans have had cataracts, often accompanied by notable night vision deficits.
- In contrast, younger individuals rarely have night blindness unless it is tied to inherited retinal conditions such as retinitis pigmentosa or congenital stationary night blindness. Retinitis pigmentosa alone affects approximately 0.03% of the U.S. population.
- Geographic Variations:
- States with older populations and fewer healthcare resources show higher rates of untreated vision problems (including night blindness). Vision loss prevalence can be nearly three times higher in certain states (e.g., West Virginia) than in those with younger or more affluent populations.
- Rural areas may face more difficulties accessing eye care, yet urban populations have higher incidences of diabetes (which can also impair vision). Overall, there is no single “hot spot” for night blindness, as it aligns with general patterns of vision impairment and resource availability.
Causes of Night Blindness
Appreciating the main causes behind nyctalopia is crucial for public health planning and individual management. This section outlines the primary factors that lead to significant difficulties seeing in low-light settings.
- Cataracts and Other Treatable Causes:
- Cataracts (clouding of the eye’s natural lens) are overwhelmingly the most common reversible cause of night blindness among seniors. Over 24 million Americans aged 40 or above have cataracts. Removing the cloudy lens typically restores normal or near-normal night vision.
- Refractive errors (especially nearsightedness) can also worsen low-light vision if undercorrected. Updating a patient’s glasses prescription or providing anti-reflective lenses often yields marked improvement.
- Vitamin A deficiency remains the classic cause of night blindness globally, but is extremely rare in the U.S. When it does occur, often in individuals with malabsorption disorders or extremely restrictive diets, supplementation rapidly resolves the problem.
- Retinal Dystrophies and Other Permanent Causes:
- Retinitis pigmentosa (RP): Estimated at about 100,000 cases nationwide, it is a progressive, inherited condition in which the rod photoreceptors degenerate, leading first to night blindness and eventually to peripheral vision loss.
- Congenital stationary night blindness is another inherited form present from birth. Although it does not typically progress, patients endure lifelong trouble seeing in dimly lit environments.
- Other retinal diseases such as choroideremia or advanced glaucoma may also compromise rod function in the retina, causing permanent or semi-permanent night vision deficits.
Trends and Shifts Over the Past Decade
Understanding how night blindness data have evolved in the last 10 years helps highlight progress in prevention and treatment.
- Stable Low Rates of Nutritional Night Blindness:
- Public health measures, vitamin fortification, and consistent access to food have kept true vitamin A deficiency at minimal levels in the U.S. This trend has remained steady.
- Instances that do arise often involve specific populations (e.g., bariatric surgery patients), who typically see near-complete reversal upon proper supplementation.
- Rising Importance of Age-Related Factors:
- As the baby boomer generation moves into retirement, the sheer number of older adults coping with eye diseases has grown. While the proportion of people with night blindness has not spiked dramatically, the total number has increased simply due to demographic shifts.
- Advances in cataract surgery have mitigated this effect somewhat, reducing the duration people remain with cloudy lenses that degrade night vision.
- Genetic Therapies on the Horizon:
- The approval of the first gene therapy for a specific form of inherited retinal disease marks a milestone. Though the therapy (voretigene neparvovec) targets one particular gene mutation, it demonstrates that even previously irreversible night blindness may be partially reversed through genetic interventions.
- Ongoing clinical trials aim to expand these therapies to other mutations, offering cautious optimism that night blindness from hereditary disorders may become more treatable in the future.
Notable Treatment Outcomes
Each main type of night blindness (treatable or otherwise) comes with unique intervention success rates and patient results. Tracking these outcomes is essential for designing effective healthcare strategies.
- Cataract Surgery
- Widely considered one of the safest and most common procedures in the U.S., cataract surgery boasts a success rate of around 95% for achieving significantly improved vision.
- Studies show that correcting cataracts can cut older drivers’ car crash rates by about 50%, underscoring how restored night vision translates directly to increased safety.
- Many patients report an immediate ability to see more clearly in dim light after surgery, helping them remain socially active and independent.
- Vitamin A Supplementation
- For those with deficiency-induced nyctalopia, high-dose vitamin A treatment yields near-total resolution of symptoms in most cases. Dark adaptation may return to normal within days of therapy.
- Preventive supplementation in at-risk groups (for instance, patients with certain malabsorption conditions) further reduces the incidence of nutritional night blindness.
- Therapies for Retinal Diseases
- High-dose vitamin A palmitate has been used for years to slow the progression of retinitis pigmentosa, delaying more severe losses in dark adaptation.
- The newly approved gene therapy for RPE65-related degenerations has restored functional night vision in many participants, representing a breakthrough. Though it applies to only a subset of inherited disorders, additional gene therapies are under development.
- Low-vision aids, orientation training, and assistive devices continue to help those whose night vision deficits are not fully correctable.
Impact on Daily Life, Safety, and Society
Numbers tell only part of the story. Night blindness also comes with profound personal, social, and economic implications.
- Driving Restrictions and Accident Risk
- Research shows 20 to 50% of older drivers self-limit or cease driving at night because of vision difficulties, sometimes leading to reduced mobility and social interactions.
- Nationwide statistics reveal that while fewer cars travel at night, around half of all traffic fatalities occur during dark hours. Impaired night vision compounds this danger.
- Treating night blindness (for instance, via cataract surgery) reduces crash risk significantly, highlighting the intersection of public safety and ocular health interventions.
- Falls and Household Safety
- Individuals with impaired night vision may trip or collide with objects in dim hallways or streets. Older adults with significant vision problems show about double the risk of falls compared to peers with normal vision.
- This increases healthcare costs, hospital admissions, and can lead to premature moves into assisted living facilities if not addressed.
- Occupational and Economic Effects
- Certain jobs that require reliable low-light vision (commercial driving, emergency response, night shifts) may be off-limits to people with severe nyctalopia.
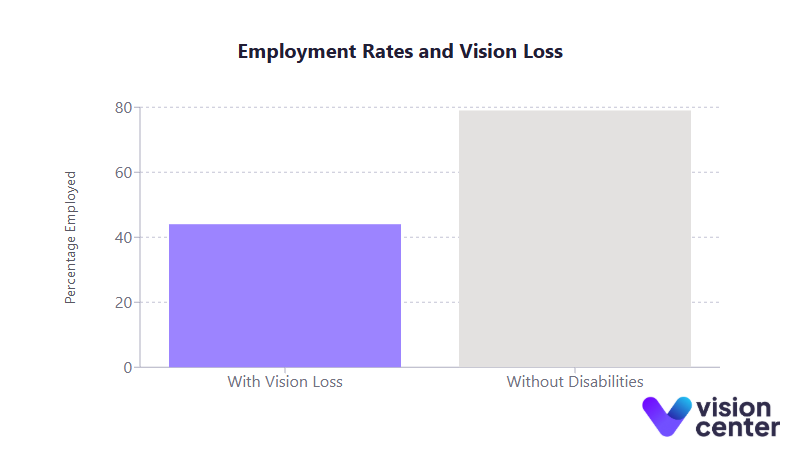
- Workers with visual impairments (including night blindness) have notably lower employment rates. Only about 44% of working-age Americans with significant vision loss are employed, compared to 79% without disabilities.
- Employers and public agencies often face additional expenses in the form of enhanced lighting, assistive technologies, and job accommodations for individuals who cannot see well at night.
- Quality of Life and Mental Health
- Social isolation can result when individuals avoid evening activities or become dependent on others for transportation in low-light conditions.
- Studies show older adults with vision impairment, including night blindness, have roughly twice the rate of depression compared to those with normal vision.
- When night blindness is treatable, successful intervention often leads to major improvements in emotional well-being, as regaining the freedom to drive or move around safely at night reopens vital aspects of daily life.
Data in Tables
For quick reference, below are two concise tables that highlight important figures:
Table 1: Major Causes of Night Blindness in the U.S. and Their Approximate Prevalence
| Cause/Condition | Estimated U.S. Prevalence | Key Night Vision Impact |
| Cataracts (age-related) | ~24 million (≥40 years old) | Leading cause of treatable night vision loss in seniors. |
| Retinitis Pigmentosa (genetic) | ~100,000 individuals (~0.03% of the population) | Progressive; early sign is difficulty seeing in the dark |
| Vitamin A Deficiency | ~0.3% of population (extremely rare cause) | Often quickly reversed via supplementation |
| Congenital Stationary Night Blindness | Very rare; exact numbers not well established | Lifelong night blindness starting in childhood |
Table 2: Selected Impact Metrics Related to Night Blindness & Vision Impairment
| Metric (Impact Area) | Statistic (U.S.) |
| Older drivers limiting night driving | 20 to 50% of seniors avoid or restrict after-dark driving |
| Post-cataract surgery crash reduction | ~50% fewer car accidents among older drivers once treated |
| Fall risk with vision impairment | ~2× higher likelihood of falls in older adults |
| Depression rate in visually impaired seniors | ~33% vs ~15% in those without vision problems |
| Employment rate for people with visual impairments | ~44% vs 79% in those without disabilities |
Night blindness in the United States, while far less common than many other forms of visual impairment, represents a critical issue for those affected. The statistical data makes clear that nyctalopia largely results from conditions like cataracts or inherited disorders, which are causes that are often either treatable or that benefit from emerging research.
This knowledge underscores the importance of regular eye care for older adults, accessible cataract surgeries, and ongoing clinical efforts to develop therapies for retinal dystrophies. Early intervention significantly improves quality of life, reducing the risk of nighttime crashes, fall injuries, and social isolation.
Where treatment is not yet available, practical adaptations and low-vision support services remain instrumental. Moving forward, the integration of gene-based therapies, continuous improvements in surgical technology, and enhanced public awareness may further reduce the burden of night blindness and help those affected maintain their independence and safety well into the future.
In this article
16 sources cited
Updated on March 25, 2025
Updated on March 25, 2025
About Our Contributors
Mara Sugue, with a B.A. in Social Sciences, is a dedicated web content writer for Vision Center. She is committed to making eye health research accessible and understandable to people from diverse backgrounds and educational levels. Her writing aims to bridge the gap between complex vision health topics and readers' needs for clear, factual information.
Dr. Melody Huang is an optometrist and freelance health writer with a passion for educating people about eye health. With her unique blend of clinical expertise and writing skills, Dr. Huang seeks to guide individuals towards healthier and happier lives. Her interests extend to Eastern medicine and integrative healthcare approaches. Outside of work, she enjoys exploring new skincare products, experimenting with food recipes, and spending time with her adopted cats.

