Updated on March 25, 2025
Statistics on Vision Health in the Elderly


Vision Center is funded by our readers. We may earn commissions if you purchase something via one of our links.
Vision health among older adults is a vital but often underestimated aspect of aging. From common conditions like cataracts and presbyopia to more complex diseases such as glaucoma and macular degeneration, vision issues affect daily life, independence, and overall well-being in the elderly population.
Over the past decade, researchers and public health organizations have amassed extensive data on how vision impairments evolve with age, the disparities in accessing care, and the growing potential of treatment and rehabilitation.
These statistics provide not only a snapshot of current realities but also a roadmap for the future. Below is a detailed examination of the numbers behind vision health in the elderly, focusing on prevalence, trends, disparities in care, outcomes of interventions, and future projections.
Key Statistics at a Glance
- By age 80, over half of Americans develop cataracts or have undergone cataract surgery.
- Glaucoma risk doubles between ages 65 and 80, affecting up to about 10% of the oldest age group.
- Nearly 25% of older adults living with diabetes develop diabetic retinopathy, a leading cause of blindness in this population.
- Vision impairment costs in the U.S. surpass $35 billion annually, including direct medical expenses, long-term care, and lost productivity.
Prevalence of Age-Related Eye Conditions
Understanding the prevalence of vision conditions is crucial to grasping the overall landscape of elderly eye health. A range of age-specific diseases (cataracts, glaucoma, macular degeneration, diabetic retinopathy, and presbyopia) collectively account for the bulk of visual impairment among older adults.
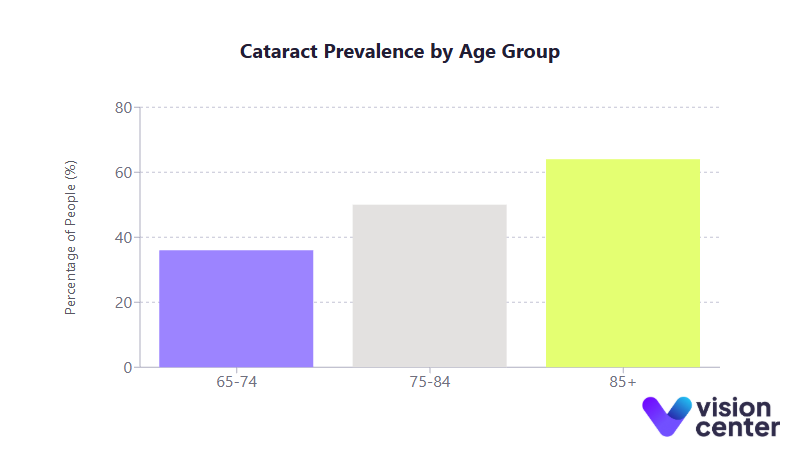
- Cataracts:
- About 24 to 36% of people between ages 65 and 74 have cataracts, climbing to 50% in those 75 to 84 and ≥64% in those 85 and older.
- Cataracts remain the leading cause of visual impairment in seniors, responsible for around half of low-vision cases.
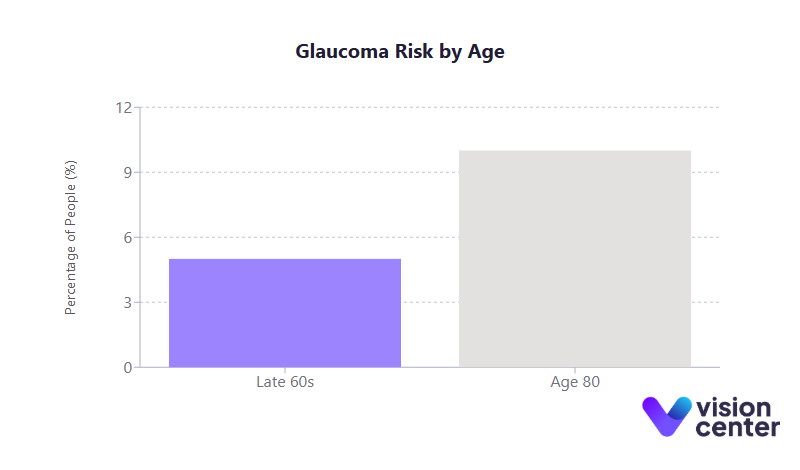
- Glaucoma:
- Approximately 5% of those in their late 60s have glaucoma, with the risk roughly doubling by age 80.
- African American and Hispanic seniors experience higher glaucoma rates than white counterparts, yet are less likely to receive timely intervention.
- Age-Related Macular Degeneration (AMD):
- AMD prevalence increases with age, affecting around 1 to 2% of people in their mid-60s and rising to ≥10% in those 85+.
- Advanced AMD can severely limit central vision, significantly impacting daily activities such as reading and driving.
- Diabetic Retinopathy:
- About 1 in 12 older adults with diabetes faces vision-threatening retinopathy.
- Poorly managed diabetes accelerates cataract formation and increases glaucoma risk, highlighting the link between systemic health and vision.
- Presbyopia (Near-Vision Decline):
- Presbyopia becomes nearly universal by the mid-60s, with the vast majority of older adults requiring reading glasses or bifocals.
- Estimates suggest 83 to 89% of those aged 45 and older are affected, with near 100% prevalence among the 65+ population.
As overall life expectancy increases, so does the likelihood of encountering multiple eye conditions. Indeed, about 1 in 4 adults over 80 experiences significant vision loss, even with corrective lenses. These patterns underscore the importance of screening, early intervention, and integrated medical care in preserving visual function for as long as possible.
Healthcare Delivery and Access
Maintaining healthy eyesight in older adulthood often depends on effective healthcare delivery (regular eye exams, timely treatments, and access to low-vision support). Yet significant disparities persist based on factors such as race, income, and geography.
Access Disparities in Vision Care
Access to preventive care and specialized vision services is uneven across demographic groups, contributing to worse outcomes for certain populations:
- Race/Ethnicity: African American and Hispanic seniors have higher rates of glaucoma and diabetic retinopathy, yet receive fewer eye care services on average. Fewer referrals for cataract surgery, low-vision aids, and regular exams amplify their risk of advanced disease.
- Socioeconomic Status (SES): Low-income seniors are more likely to go without routine vision check-ups. Roughly 23% of visually impaired older adults cite cost or lack of insurance as the top barrier to care, a challenge aggravated by Medicare’s limited coverage for routine exams and glasses.
- Geographic Factors: Rural areas often have fewer eye specialists, leading to lower rates of preventive care like dilated eye exams and cataract surgery. Transportation hurdles further constrain these seniors’ ability to access timely interventions.
Because eye diseases can progress silently, particularly glaucoma, delayed care frequently results in preventable vision loss. Improving the coverage and availability of eye care services is a core priority in addressing these inequities.
Support Services and Rehabilitation Utilization
Low-vision rehabilitation and assistive services substantially improve day-to-day functioning for those with chronic vision loss. However, utilization remains notably low:
- Only about 4.3% of eligible older adults receive specialized vision rehab support, such as training with magnifiers, contrast enhancements, and mobility aids.
- Rates of low-vision device usage and vision rehabilitation are even lower for minority groups, exacerbating existing outcome disparities.
- Referrals to these services are often underemphasized by primary providers, leaving many seniors unaware of available resources.
Expanding rehabilitation services, both within clinical settings and community programs, can make a critical difference, helping older adults with significant vision impairments maintain independence and reduce the need for residential care.
Preventive Care and Early Detection Programs
Routine eye exams and screening initiatives are key to catching asymptomatic or progressive diseases before irreversible damage occurs:
- Annual Eye Exams: Recommended especially for diabetics and those at high risk for glaucoma.
- Glaucoma Screening: Often described as the “silent thief of sight,” glaucoma can remain undiagnosed until substantial vision loss has occurred. Up to 50% of those affected are unaware they have it.
- Diabetic Retinopathy Screenings: Yearly retinal photographs can help identify early changes and prompt laser or injection therapy. Proper diabetes and blood pressure management substantially reduce the risk of severe complications.
- AMD Awareness Campaigns: High-dose antioxidant supplements and early detection efforts have slowed the progression of AMD in many patients, improving long-term preservation of central vision.
Although the benefits of large-scale vision screening in asymptomatic older adults are sometimes debated, the consensus is that high-risk individuals (those with diabetes, a family history of glaucoma, or other known risk factors) should have comprehensive, regular exams. Community outreach efforts, including free or subsidized screenings, have led to earlier detection in underserved regions.
Intervention Effectiveness and Outcomes
Medical and surgical interventions for age-related eye conditions have advanced significantly in recent decades. For many older adults, these treatments are transformative, restoring or stabilizing vision that might otherwise deteriorate.
Treatment Success for Major Eye Conditions
- Cataract Surgery:
- Boasts a 95%+ success rate in improving visual acuity.
- Serious complications are rare, and most patients experience sustained benefits.
- Studies show lower rates of hip fractures, car crashes, and even reduced mortality among older adults who undergo timely cataract removal.
- Glaucoma Management:
- First-line therapy typically involves pressure-lowering eye drops to slow disease progression. Laser procedures (trabeculoplasty) or surgical options are employed if medications are insufficient.
- Minimally invasive glaucoma surgeries (MIGS) have grown in popularity, especially when combined with cataract surgery in older adults.
- Age-Related Macular Degeneration:
- Anti-VEGF injections help preserve vision in over 90% of wet AMD cases and can improve sight for about one-third of patients.
- High-dose vitamin supplementation has been shown to delay progression in those with risk factors for advanced AMD.
- Diabetic Retinopathy:
- Tight blood sugar and blood pressure control, alongside laser photocoagulation or anti-VEGF injections for macular edema, significantly reduce blindness risk.
- Early intervention correlates with a >50% reduction in severe vision loss.
These approaches underscore that while many conditions remain chronic, their course can be altered substantially if caught and treated early.
Surgical Interventions and Trends
Surgical treatments have also grown in scope and number:
- Rising Cataract Surgery Rates:
- With enhanced safety and outcomes, more older adults opt for surgery in their late 60s or 70s rather than waiting for advanced cataracts.
- Even patients in their 80s and 90s see meaningful improvements in vision and quality of life.
- Combination Treatments:
- Ophthalmologists frequently pair cataract procedures with glaucoma surgeries (e.g., MIGS devices) for those with coexisting conditions, reducing the overall treatment burden.
- Retinal Procedures:
- Intravitreal injections for AMD or diabetic retinopathy have skyrocketed over the past 10 years, becoming routine care to stabilize or improve retinal health.
- Proactive laser treatments help minimize the risk of advanced proliferative disease in diabetic patients.
The cumulative effect of these innovations has significantly lowered the likelihood of irreversible blindness from conditions that were once untreatable or poorly controlled.
Long-Term Outcomes and Functional Improvement
Many seniors benefit from lasting improvements:
- Cataract Surgery: Most older adults report not just better vision but also enhanced mobility and daily functioning.
- Glaucoma Treatments: Although the disease is lifelong, modern therapies and vigilant monitoring allow many patients to retain usable vision.
- Retinal Diseases: Anti-VEGF for wet AMD and diabetic macular edema can preserve central vision for years, enabling reading, driving, and other independent activities.
- Ongoing Maintenance: Frequent follow-up is typically required (e.g., regular injections for AMD, consistent drop regimens for glaucoma), but the payoff in preserved vision is substantial.
Collectively, these interventions are increasingly viewed not just as sight-saving but also as vital for maintaining seniors’ autonomy and overall well-being.
Patient Outcomes and Quality of Life
Vision impairment in old age carries far-reaching repercussions for mental health, social engagement, and the capacity to live independently.
Financial Burden and Cost of Care
- Insurance Gaps: While Medicare covers medically necessary eye surgeries and certain treatments, it typically does not cover routine eye exams or corrective lenses. This forces many elderly individuals to pay out-of-pocket for basic vision care.
- Out-of-Pocket Expenses: Eyeglasses, low-vision aids, and specialist visits can become prohibitively expensive for those on fixed incomes. Around 39 to 40% of older adults postpone or skip eye appointments because of cost concerns.
- Societal Costs: The annual U.S. burden of adult vision disorders exceeds $35 billion in direct medical expenses, long-term care, and productivity losses. Preventive measures and timely treatments could potentially offset a portion of these broader economic impacts.
Quality of Life Impacts (Mobility, Mental Health, Social Engagement)
- Increased Fall Risk: Seniors with compromised vision are significantly more likely to experience falls and fractures. Fear of falling can also lead to reduced physical activity and further isolation.
- Depression and Anxiety: Vision loss doubles or even triples the likelihood of depression, with conditions like advanced AMD strongly linked to higher rates of depressive symptoms.
- Social Isolation: Impaired ability to drive, read, or recognize faces can make older adults withdraw from social gatherings. Many report loneliness and a fear of dependency, underscoring the emotional toll of vision decline.
- Positive Effects of Intervention: Cataract removal, refractive correction, and low-vision rehabilitation each correlate with better mobility, social participation, and mental health, highlighting the importance of accessible treatments.
Vision and Independent Living
- Higher Rates of Institutionalization: Older adults with significant vision impairment are around 3× more likely to live in nursing homes, and more than half of long-term care residents exhibit some level of vision loss.
- Functional Decline: Even moderate vision impairment markedly increases difficulty in activities of daily living (ADLs) such as cooking, medication management, and household tasks.
- Preventing or Delaying Institutional Care: Timely cataract surgery, proper glaucoma/AMD management, and in-home adaptations can enable many seniors to remain safely in their own homes for years longer.
- Economic Benefits: Prolonging independence through effective vision interventions can reduce long-term care costs, benefiting not only individuals but also healthcare systems.
Future Projections and Trends
With the aging Baby Boomer generation, the burden of age-related eye disease is poised to grow substantially, but ongoing innovations also hold promise for reducing vision loss.
Projected Prevalence and Demographic Shifts
- Population Aging: By 2050, the number of Americans 65 and older will nearly double, causing a steep rise in eye conditions such as AMD, glaucoma, and diabetic retinopathy.
- Forecasted AMD Cases: Projections indicate AMD could affect ~5.4 million Americans by 2050, more than doubling its current prevalence.
- Minority Populations: As the proportion of Black and Hispanic seniors increases, so will the prevalence of glaucoma and diabetic eye disease, amplifying existing disparities if not addressed.
- Doubling of Vision Impairment: Some estimates suggest that the overall number of visually impaired older adults will climb from around 12 to 13 million today to over 27 million by 2050.
Treatment Advancements on the Horizon
- Gene and Stem Cell Therapies: Research aims to repair or replace damaged retinal cells in diseases like AMD, potentially restoring lost vision.
- Longer-Acting Medications: Extended-release implants and more potent drug formulations could reduce the need for frequent injections in conditions like AMD and diabetic retinopathy.
- Glaucoma Innovations: Neuroprotective treatments and newer surgical implants may further slow or halt optic nerve damage.
- Assistive Technology: Smart glasses, AI-driven navigation apps, and voice-interactive devices promise greater autonomy for older adults with partial sight.
Given the anticipated surge in the senior population, experts emphasize integrating vision services into broader geriatric care, focusing on both prevention and cutting-edge treatments. Advancements in early detection, combined with emerging therapies, may ultimately reshape how society manages and perceives vision health in older age.
In the coming years, these collaborative efforts, from research breakthroughs to public health outreach, can help ensure more elderly individuals maintain functional vision and an improved quality of life.
In this article
19 sources cited
Updated on March 25, 2025
Updated on March 25, 2025
About Our Contributors
Mara Sugue, with a B.A. in Social Sciences, is a dedicated web content writer for Vision Center. She is committed to making eye health research accessible and understandable to people from diverse backgrounds and educational levels. Her writing aims to bridge the gap between complex vision health topics and readers' needs for clear, factual information.
Dr. Melody Huang is an optometrist and freelance health writer with a passion for educating people about eye health. With her unique blend of clinical expertise and writing skills, Dr. Huang seeks to guide individuals towards healthier and happier lives. Her interests extend to Eastern medicine and integrative healthcare approaches. Outside of work, she enjoys exploring new skincare products, experimenting with food recipes, and spending time with her adopted cats.

