Updated on March 25, 2025
Diabetic Retinopathy Statistics


Vision Center is funded by our readers. We may earn commissions if you purchase something via one of our links.
Diabetic retinopathy is a leading cause of vision loss for working-age adults. It occurs when chronically high blood sugar damages the small blood vessels in the retina, threatening sight.
Over the last decade, ongoing research and public health data have shed new light on the prevalence, risk factors, and treatment outcomes for this condition, revealing both improvements in prevention and persistent gaps in care.
Diabetic retinopathy statistics are part of a broader picture of diabetes-related complications. National surveys, clinical studies, and healthcare cost analyses highlight the increasing size of the diabetes population, underscore the importance of early detection, and demonstrate the impact of improved treatments.
Understanding these numbers not only helps clinicians and policymakers allocate resources but also empowers individuals with diabetes to prioritize regular eye exams and comprehensive disease management.
Key Statistics at a Glance
- About one in four adults with diabetes develops some form of diabetic retinopathy, affecting millions of Americans each year.
- Roughly 5% of people with diabetes have vision-threatening retinopathy, conditions like proliferative retinopathy, or severe macular edema.
- Screening rates remain suboptimal: approximately one-third of U.S. adults with diabetes do not receive the recommended annual eye exam.
- Racial disparities persist: Black and Hispanic adults with diabetes are nearly twice as likely as white adults to have sight-threatening diabetic retinopathy.
Epidemiology and Prevalence
Why these data matter: Gauging how common and widespread diabetic retinopathy is helps healthcare providers, public health officials, and patients understand the scope of the problem and tailor interventions effectively.
- Overall Burden:
- The United States has seen a rise in the number of people with diabetic retinopathy as the diabetes epidemic continues. Recent estimates place the total at nearly 10 million Americans living with some level of retinopathy.
- Within the diabetes population, about 25% to 30% experience retinopathy, while around 5% have advanced or vision-threatening forms.
- Trends Over Time:
- As diabetes has grown more prevalent over the past two decades, the absolute number of retinopathy cases has climbed steadily.
- Despite this increase, improvements in care have modestly lowered the proportion of people with diabetes who progress to severe stages. However, the total count of affected individuals continues to rise because of the expanding diabetes population.
- Age and Duration of Diabetes:
- Retinopathy rates escalate with age and with longer duration of diabetes.
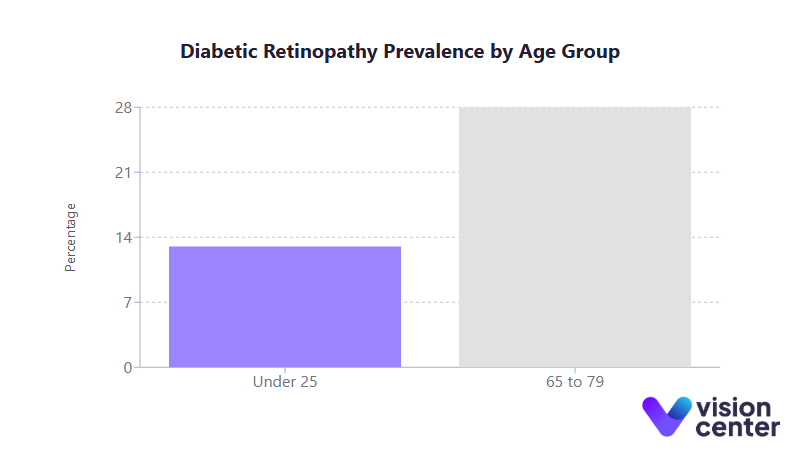
- Among younger individuals with diabetes (under 25), the prevalence of retinopathy can be as low as 13%. For seniors with diabetes (65 to 79), it approaches 28% or more.
- Type 1 diabetes, often diagnosed in childhood or adolescence, historically carries a particularly high long-term risk if blood sugar is not well controlled.
- Racial and Ethnic Disparities:
- Black and Hispanic adults with diabetes experience nearly double the rate of vision-threatening retinopathy compared to white adults.
- Socioeconomic factors compound these differences: communities with limited access to healthcare, lower educational attainment, or higher poverty levels see higher retinopathy rates.
- Geographic Patterns:
- States with high obesity and diabetes rates, especially in the South, tend to have greater prevalence of diabetic retinopathy among their diabetic populations.
- Certain regions report prevalence rates among adults with diabetes exceeding 30%, while others remain closer to 20%.
The Importance of Early Detection
Why these data matter: Catching diabetic retinopathy in its earlier stages often means preserving sight and reducing the need for costlier interventions down the road.
- Screening Guidelines and Gaps:
- An annual dilated eye exam is recommended for all individuals with diabetes, yet only about 65% follow through each year.
- Among Medicare beneficiaries with diabetes, screening rates in some states remain below 50%. Even though Medicare typically covers the cost of an eye exam for diabetes, disparities in both rural and urban settings indicate transportation, insurance nuances, and awareness issues still create barriers.
- Telemedicine and Community Programs:
- Tele-retinal screening has proven effective in increasing detection rates. Primary care clinics can capture retinal images and transmit them to eye specialists for review, reducing the travel and wait times for patients.
- Community outreach efforts, such as free or subsidized vision screenings in underserved areas, have successfully identified significant numbers of patients with previously undiagnosed diabetic retinopathy.
- Impact of Early Detection:
- When retinopathy is caught in mild or moderate stages, treatments can prevent progression in a vast majority of cases.
- Public health data suggest that consistent screening and timely treatment could avert up to 95% of severe vision loss cases linked to diabetic retinopathy.
Advances in Treatment and Prevention
Why these data matter: Tracking which interventions are most effective allows patients and providers to choose the best strategies for preserving vision and quality of life.
- Pharmacologic Breakthroughs:
- Anti-VEGF medications (injected into the eye) revolutionized the management of diabetic macular edema and proliferative diabetic retinopathy, often stabilizing or improving vision.
- Laser therapy (pan-retinal photocoagulation) remains a mainstay, especially for proliferative disease. But many patients now benefit from combined or standalone injection therapies that can lead to better central vision outcomes.
- Glycemic and Blood Pressure Control:
- Good overall diabetes management (maintaining near-normal blood sugar and healthy blood pressure levels) has been shown to reduce the onset of retinopathy by more than half.
- Data from long-term studies confirm that each percentage point reduction in hemoglobin A1c significantly lowers the risk of developing or worsening diabetic retinopathy.
- Public Health and Prevention Programs:
- The National Diabetes Prevention Program (NDPP) and various self-management education initiatives emphasize intensive lifestyle interventions to delay or prevent diabetes.
- For those already diagnosed, diabetes self-management programs encourage tight glucose and blood pressure control, screening reminders, and specialist referrals, all of which reduce retinopathy complications.
- Reduced Risk of Blindness:
- With modern treatments, the likelihood of progression to severe vision loss or blindness has dropped substantially.
- Among individuals receiving consistent care, the prognosis is excellent: most maintain functional vision throughout their lives, underscoring how transformative current approaches can be when applied regularly and equitably.
Healthcare Delivery, Costs, and Disparities
Why these data matter: Understanding economic and access challenges helps highlight why many patients still slip through the cracks, despite the availability of sight-saving treatments.
- Economic Burden:
- Diabetes overall costs hundreds of billions of dollars annually in the United States. Eye-related complications, including diabetic retinopathy, add hundreds of millions more to direct and indirect costs.
- Individuals with retinopathy often have higher overall healthcare expenditures than those with diabetes but no eye complications, reflecting the need for multiple visits, potential surgeries, injections, and vision aids.
- Insurance Coverage and Access to Specialists:
- While most insurance plans, including Medicare, cover diabetic eye exams, cost-sharing or logistical barriers (e.g., transportation, provider shortages) still impede access.
- Rural and low-income communities are disproportionately affected by shortages in optometry or ophthalmology services, leading to lower screening rates and, in turn, worse outcomes.
- Ongoing Disparities:
- Nationwide, Black and Hispanic adults with diabetes have lower screening rates and higher prevalence of advanced retinopathy compared to white adults.
- Some states focus on telemedicine and mobile vision clinics to address these disparities, but consistent funding and health system alignment remain critical to ensure all communities can benefit.
Patient Outcomes and Quality of Life
Why these data matter: Beyond statistics, diabetic retinopathy affects individuals’ daily lives, independence, and mental well-being.
- Vision-Related Quality of Life:
- Even moderate diabetic retinopathy can impair activities like reading, driving at night, and recognizing faces. Patients with advanced retinopathy often report significant anxiety over potential vision loss.
- Studies using standardized surveys show that people with vision-threatening diabetic retinopathy score markedly lower on visual function and quality of life measures compared to those without retinopathy.
- Long-Term Prognosis:
- With timely treatment, an estimated 90% or more of patients diagnosed with proliferative retinopathy can avoid blindness.
- Intensive glucose management early in the course of diabetes confers lasting benefits, a phenomenon sometimes referred to as “metabolic memory.” Conversely, poor control at any stage of diabetes increases the likelihood of vision-related complications.
- Major Risk Factors:
- Longer duration of diabetes, persistently high blood sugar, elevated blood pressure, and overlapping microvascular complications (such as kidney disease) all accelerate retinopathy progression.
- Tight control of these factors is linked to fewer eye-related complications and better vision outcomes.
Final Summary
Over the last decade, diabetic retinopathy research has underscored both the scope and urgency of this vision-threatening complication. Millions of Americans now face varying degrees of retinopathy, driven by rising diabetes prevalence.
From a public health perspective, the data confirm that prevention and early detection work: even as the overall number of Americans with diabetes grows, rigorous management and timely intervention can keep a vast majority of them free from severe vision loss.
Going forward, increasing access to eye exams, addressing racial and geographic disparities, and integrating diabetes care with vision health services remain key priorities. By continuing to expand effective programs and treatments, healthcare providers and policymakers can empower individuals with diabetes to preserve their sight and maintain a high quality of life.
In this article
8 sources cited
Updated on March 25, 2025
Updated on March 25, 2025
About Our Contributors
Mara Sugue, with a B.A. in Social Sciences, is a dedicated web content writer for Vision Center. She is committed to making eye health research accessible and understandable to people from diverse backgrounds and educational levels. Her writing aims to bridge the gap between complex vision health topics and readers' needs for clear, factual information.
Dr. Melody Huang is an optometrist and freelance health writer with a passion for educating people about eye health. With her unique blend of clinical expertise and writing skills, Dr. Huang seeks to guide individuals towards healthier and happier lives. Her interests extend to Eastern medicine and integrative healthcare approaches. Outside of work, she enjoys exploring new skincare products, experimenting with food recipes, and spending time with her adopted cats.

