Updated on October 21, 2024
Papilledema (Swollen Optic Nerve)


Vision Center is funded by our readers. We may earn commissions if you purchase something via one of our links.
What is Papilledema?
The optic nerve (also called the second cranial nerve or CNII) transmits visual information from the eyes to the brain.
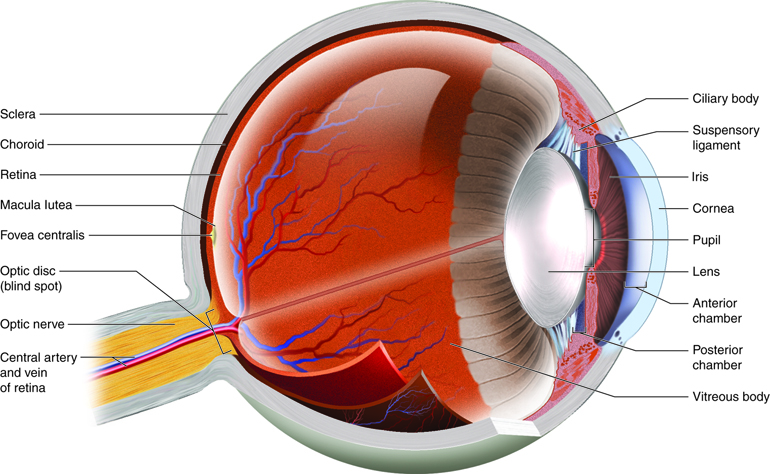
Papilledema or papilloedema is the swelling of the optic disc or the part of the optic nerve located inside the eye.
It is caused by intracranial hypertension (IH) or increased pressure within and around the brain.
Papilledema can develop within hours or weeks, depending on the underlying cause. It is usually bilateral and affects both eyes.
In rare cases, it has a unilateral presentation and affects one eye.
Papilledema or optic nerve swelling indicates the presence of a serious and often life-threatening condition.
Unless treated, elevated brain pressure can lead to permanent nerve damage, vision loss, and death.1
Is optic disc edema the same as papilledema?
No. Papilledema is not the same as optic disc edema. While both lead to optic disc swelling, they have different causes:
- True papilledema: Results from increased brain pressure due to an underlying condition
- Optic disc edema: Also known as pseudopapilledema, it is caused by optic nerve damage
Their symptoms also vary. Papilledema commonly affects your peripheral vision. It does not change your central vision and visual acuity until later.
Optic disc edema affects your central visual field at the onset, reducing your ability to distinguish objects and shapes.2
Signs and Symptoms of Papilledema
Papilledema often begins with temporary vision changes.
You may experience blurred or double vision, flickering eyesight, or complete vision loss for several seconds at a time.
Some people may not initially have changes in vision. But you can watch for signs of raised intracranial pressure:
- Nausea
- Vomiting
- Headache
Projectile vomiting is a sign of elevated ICP. It causes you to forcefully expel stomach contents up to several feet away.
You can also monitor for Cushing's Triad. It refers to a set of signs that indicate increased pressure in the brain, namely:
- Decreasing heart rate
- Irregular breathing
- Widening pulse (or an increasing difference between the systolic and diastolic blood pressure)
Papilledema due to increased cerebrospinal fluid may lead to pulsatile tinnitus.
Pulsatile tinnitus is characterized by rhythmic sensations in one or both ears. These include thumping, whooshing, and throbbing that sync with the heartbeat.
Headaches usually worsen upon waking, while lying down, or when straining. Despite the headaches, papilledema does not cause eye pain.
People with severe papilledema may experience:
- Decreasing visual acuity
- Impaired color perception
- Limited visual field
What Causes Papilledema?
Papilledema can be caused by a variety of diseases, injuries, and conditions that increase intracranial pressure (ICP).
In general, any brain lesion that occupies space or causes cerebrospinal fluid (CSF) to accumulate can raise your brain pressure.
Infections that cause swelling of the brain and brain tissues may also lead to bilateral papilledema.
Some known causes of papilledema are:
- Brain tumor
- Brain abscess
- Head trauma
- Brain aneurysm
- Stroke
- Hydrocephaly
- High blood pressure
- Brain hemorrhage
- Cerebral edema
- Craniosynostosis
- Meningitis
- Encephalitis
- Cerebral venous thrombosis (CVT)
Certain medications can elevate your ICP as a side effect.
These include tetracycline, lithium, minocycline, nalidixic acid, corticosteroids, and some anti-hypertensive drugs such as nitroprusside, nitroglycerine, hydralazine, and nicardipine.
Unilateral papilledema is caused by an optic nerve glioma. It is a slow-growing tumor that increases ICP in 27% of cases.3
Sometimes, the cause of increased brain pressure is unknown. This is called idiopathic intracranial hypertension (IIH) or pseudotumor cerebri.
IIH mimics a brain tumor, so you will exhibit signs of papilledema.
Risk factors for papilledema
Papilledema is a rare optic nerve disorder. It can affect anyone regardless of age, gender, race, or ethnicity.
However, idiopathic intracranial hypertension (IIH) can increase your risk for papilledema.
IIH occurs in 1 out of 100,000 Americans. Obese women in their childbearing years (aged 15 to 44) are also 20 times more likely to develop the condition.
Obesity and sudden weight gain (at least 5 to 15% of your body weight) put you at risk for idiopathic intracranial hypertension and papilledema.4
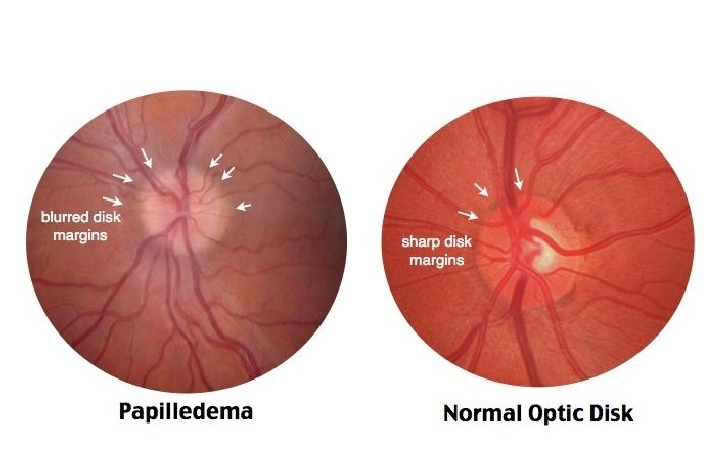
Papilledema Diagnosis
The doctor will take your medical history, vital signs, and your height and weight. They will also try to see if you have been experiencing symptoms.
Doctors can use this information to identify risk factors and potential causes of papilledema. Sometimes, it's all they need to diagnose and rule out optic nerve disorders.5
To confirm your diagnosis, an ophthalmologist may perform tests and request that you undergo additional imaging and lab tests.
Tests that can help diagnose papilledema include:
- Fundus exam
- Perimetry
- Optic coherence tomography
- Fluorescein angiography
- B-scan ultrasonography
- Computed tomography (CT) scan
- Magnetic resonance imaging (MRI)
- Magnetic resonance venography (MRV)
- Stereo color photography
- Lumbar puncture or spinal tap
Besides checking for optic nerve swelling, these tests can help your doctor find out what is causing it.
If papilledema is present, an eye specialist may use the Frisén scale to score the severity of your condition.
Listen In Q&A Format
Papilledema: Swollen Optic Nerve
Vision Center Podcast
Complications of Papilledema
Failure to decrease the ICP can also lead to complications. The health consequences will depend on the underlying cause.
For example, increased intracranial pressure caused by a brain hemorrhage leads to an aneurysm or a stroke.
But if a brain abscess causes it, the possible complications are meningitis, thrombosis, and septicemia.
Some causes of papilledema require immediate treatment. If it is not addressed soon enough, it can cause death.
Is Papilledema Permanent or Reversible?
Without treatment, intracranial hypertension will apply increasing pressure to the optic nerve and cause permanent damage.
In turn, this can lead to vision loss.
Early treatment can prevent these complications.
The success of papilledema treatment depends on proper diagnosis. If your doctor does not find the exact cause, its symptoms may return.
Papilledema Treatment & Management
Treatment requires the involvement of an ophthalmologist, a neurologist, and a neurosurgeon.
Together, they will focus their care on treating the increased intracranial pressure and relieving optic disc swelling.6
Below are some general guidelines for treating papilledema:
Medications
If you are taking drugs that raise ICP, they have to stopped or replaced. The doctor may also prescribe these medications:7
- Antibiotics: Treat brain infection
- Anticoagulants: Dissolve blood clots
- Corticosteroids: Reduce inflammation
- Pain relievers: Manage or reduce headaches
- Diuretics: Reduce brain pressure
- Carbonic anhydrase inhibitors: Decreases CSF production
Topiramate (Topamax) can provide symptomatic relief of migraines and seizures. They can also decrease ICP.
People with idiopathic intracranial hypertension can use topiramate to help with weight loss.
Surgery
Your doctor may recommend the following procedures to decrease brain pressure:6
- Lumbar puncture: Decreases cerebrospinal fluid
- Brain shunt: Redirects cerebrospinal fluid
- Optic nerve sheath decompression: Relieves optic disc swelling and worsening vision problems
If you have IIH and obesity is a risk factor, bariatric surgery may be given as an option for weight loss.
But if the raised ICP is caused by abscess or a brain tumor, a surgeon may perform burr-hole aspiration or craniotomy.
How do I bring down my ICP?
Besides seeking treatment, there are a few things you can do to manage your papilledema and ICP.
For instance, you want to avoid laying down flat on the bed. This can increase your brain pressure and worsen your symptoms.
One study shows that elevating the bed by at least 30 degrees significantly decrease ICP.8
In this article
8 sources cited
Updated on October 21, 2024
Updated on October 21, 2024
About Our Contributors
Anthony Armenta, a graduate in International Relations from the University of California, Irvine, has dedicated the past 5 years to freelance health content writing and medical editing in Barcelona. Working with public hospitals, he covers various medical specialties, including infectious diseases and pneumology. Anthony's commitment to creating fact-driven, health-related content is driven by his belief in the power of information to empower individuals to improve their health, including in areas like vision care.
Dr. Melody Huang is an optometrist and freelance health writer with a passion for educating people about eye health. With her unique blend of clinical expertise and writing skills, Dr. Huang seeks to guide individuals towards healthier and happier lives. Her interests extend to Eastern medicine and integrative healthcare approaches. Outside of work, she enjoys exploring new skincare products, experimenting with food recipes, and spending time with her adopted cats.

