Updated on October 21, 2024
What is Iridocyclitis?


Vision Center is funded by our readers. We may earn commissions if you purchase something via one of our links.
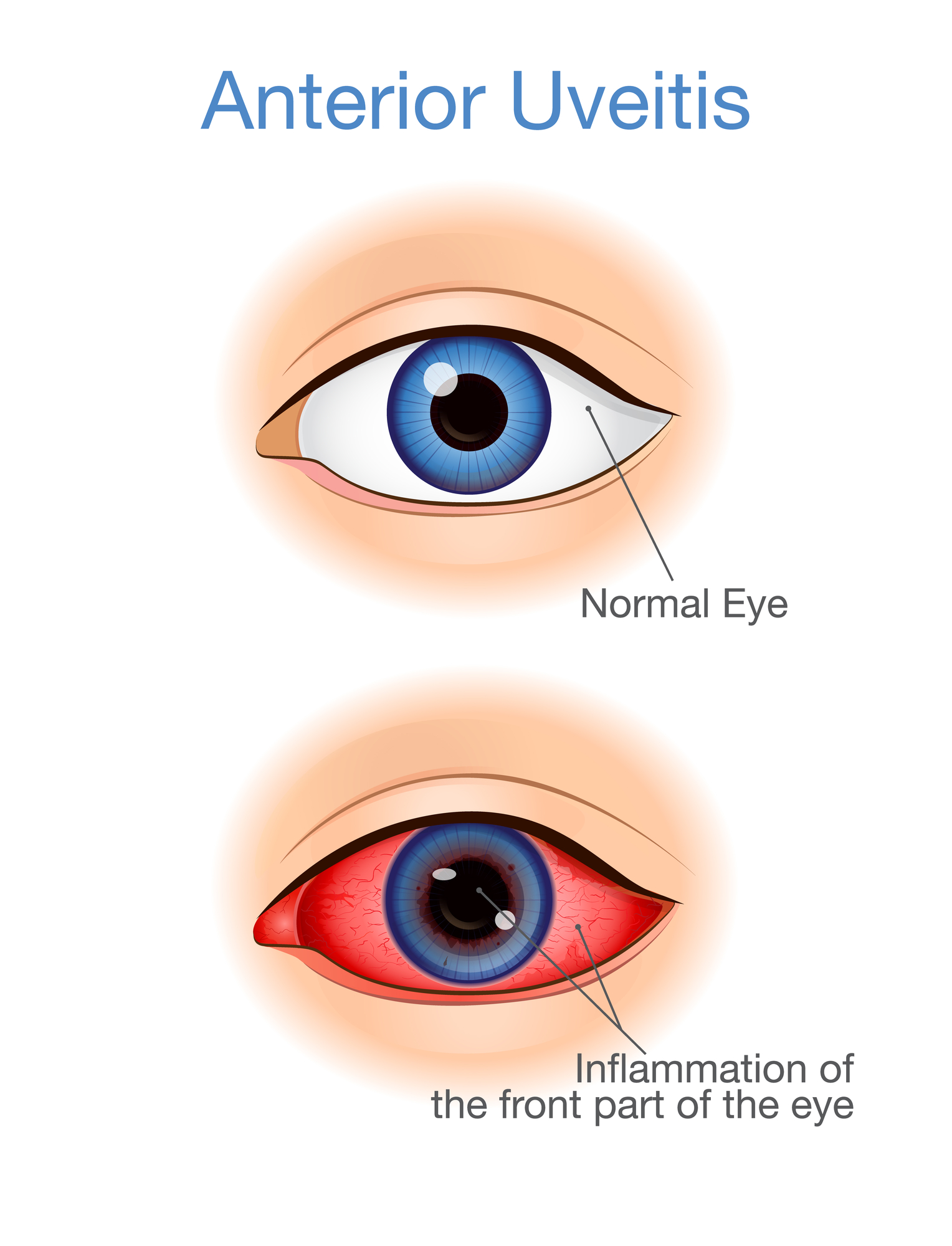
Iridocyclitis is a type of anterior uveitis.1 Uveitis is an inflammatory condition that affects the middle layer of the eye, also known as the uvea. The uvea consists of:
- Iris. The colored part of the eye.
- Choroid. The part connecting the retina to the sclera.
- Ciliary body. It helps the lens to focus.
Iridocyclitis occurs when inflammation affects the iris and the ciliary body. If only the iris is affected, the condition is known as iritis.
Iridocyclitis causes eye pain, redness, blurred vision, and sensitivity to light. If left untreated, it can lead to cataracts, uveitic glaucoma, irregular pupil, scarring, and vision loss.2
Types of Iridocyclitis
Iridocyclitis can affect one or both eyes. Symptoms last a few weeks to 3 months, depending on severity. The three types of iridocyclitis include:
- Acute iridocyclitis. Sudden inflammation of the iris and ciliary body (lasts about 4 to 8 weeks).3
- Chronic iridocyclitis. Persistent inflammation (lasts more than 3 months and recurs after treatment).
- Recurrent iridocyclitis. Frequent relapse and remission.
What are the Symptoms of Iridocyclitis?
People with iridocyclitis may experience the following symptoms:
- Pain in the eye
- Red eyes (especially around the iris)
- Blurred vision
- Headaches
- Miosis (constricted pupils)
- Photophobia (Sensitivity to light)
Untreated iridocyclitis can cause vision loss. Seek immediate medical attention if you experience the above symptoms.
How Common is Iridocyclitis?
Uveitis is rare in the United States, with an incidence of 52.4 cases per 100,000 persons/year and a prevalence rate of 115.3 per 100,000 persons.4 This condition and related complications account for about 10% of blindness cases in the United States.5
Anterior uveitis, which includes iridocyclitis and iritis, is the most common form of eye inflammation. There are fewer cases of iridocyclitis than of iritis.
Iridocyclitis can affect people of all ages but is prevalent among the middle-aged or older population.
What Causes Iridocyclitis?
The exact cause of iridocyclitis is unknown. Sometimes it can result from eye trauma, infections, and systemic diseases.
Traumatic Iridocyclitis
Eye injuries, such as a poke in the eye, chemical burns, or blunt force trauma, can cause traumatic iridocyclitis.6
The swelling and inflammation will likely subside in a few weeks as the eye heals. However, an eye exam is recommended to check for severe damage to the eye, which may pose a risk to your eyesight.
Non-Traumatic Iridocyclitis
As the name suggests, non-traumatic iridocyclitis results from anything other than eye trauma—infectious diseases, certain conditions, medications, etc.
Risk Factors for Iridocyclitis
The risk of developing iridocyclitis is high in people with the following:
1. Infections
- Viral infections such as eye shingles and herpes simplex virus (HSV).
- Bacterial infections such as syphilis (by Treponema pallidum), tuberculosis (TB), and Lyme disease (by Borrelia burgdorferi).
- Parasitic infections such as toxoplasmosis, caused by T. gondii.
- Sexually transmitted infections. Examples include syphilis and Herpes simplex virus (HSV).
2. Adverse Reactions to Medication
Some medications may negatively react with your body causing iridocyclitis. Potential culprits include oral contraceptives, interleukin-2, interleukin-6, and pamidronic acid (disodium pamidronate).7
3. Autoimmune Diseases
In people with autoimmune disorders, the immune system attacks healthy cells and can affect the eye as well.
The conditions include:8, 9
- Ankylosing spondylitis (seen in 20% to 30% of patients)
- Sarcoidosis (25% to 50%)
- Inflammatory bowel disease (IBD)
- Juvenile rheumatoid arthritis/juvenile idiopathic arthritis (JRA/JIA)
- Reactive arthritis
- Crohn’s disease
4. Weak Immune System
A weak immunity may result from conditions such as HIV/AIDS, some cancers, diabetes, and many others which cause the destruction of immune system cells, increasing the risk of infections such as iridocyclitis.
5. Smoking Habits
Prolonged exposure to smoke is dangerous to the eyes. Research shows that smokers are 2.2 times more likely to develop eye inflammation than non-smokers.10
6. Specific Genetic Variation
Although iridocyclitis (anterior uveitis) is not inherited, it’s associated with a gene called human leukocyte antigen B27, or HLA-B27. Scientists have found the HLA-B27 gene in people with autoimmune conditions, including ankylosing spondylitis and ulcerative colitis.11
Listen In Q&A Format
What is Iridocyclitis
Vision Center Podcast
When to See Your Eye Doctor
If you notice any sign of ocular inflammation, consult your eye doctor immediately for assessment and proper treatment.
Prompt testing and treatment is the best way to prevent or reduce the chances of vision loss.
How is Iridocyclitis Diagnosed?
Your doctor will ask about your medical history and perform a dilated eye exam. They will use dilating eye drops to widen your pupils and observe for signs of damage, redness, or discharge. They will also check your visual acuity, pupil response, and eye pressure, which can be affected by iridocyclitis.
A slit lamp examination may reveal aqueous flare or hypopyon (layers of white blood cells in the anterior chamber), characteristic of acute anterior uveitis.12
If your doctor suspects an underlying problem, they may order other laboratory tests and radiology to identify the root cause of your iridocyclitis.
Treatment for Iridocyclitis
Despite the possible dangers of iridocyclitis, you can fully recover if you seek immediate treatment. Treatments help reduce inflammation, manage pain, prevent complications, and restore good visual function.
Treatment of iridocyclitis may consist of:
- Topical steroids. Reduce eye inflammation. Examples include prednisolone acetate and betamethasone.
- Oral and systemic NSAIDs. Reduce frequent flare-ups of recurrent iridocyclitis.
- Anticholinergics such as atropine and cyclopentolate. Block nerve signals for pain and prevent the lens from sticking to the iris (posterior synechiae).
- Immunosuppressants like methotrexate or azathioprine slow the immune activity, especially in JIA-associated iridocyclitis.
- Antibiotics help in cases of bacterial infection, such as syphilis.
- Tumor necrosis factor-alpha (TNF-α) inhibitors. The main treatment for ankylosing spondylitis (AS), that reduces the incidence of iridocyclitis.13
- Surgery. Recommended for structural complications like secondary glaucoma, cataracts, and retinal detachment (RD).14
Regular checkups are important during the course of treatment. An imaging technique known as resting-state functional magnetic resonance imaging (fMRI) can be used to visualize changes in brain activity due to iridocyclitis and is useful in disease management.15
Summary
- Iridocyclitis (anterior uveitis) is the most common type of uveitis.
- The exact cause of iridocyclitis is unknown, but it sometimes results from eye trauma, infection, or an underlying condition.
- Most noninfectious iridocyclitis cases are mild and resolve within a few weeks.
- Common symptoms include eye pain, photophobia, eye redness, headache, and blurry vision.
- Early treatment is required to reduce the risk of structural damage and vision loss.
- Treatment for iridocyclitis may include corticosteroids, antibiotics, immunosuppressants, anticholinergics, etc.
In this article
15 sources cited
Updated on October 21, 2024
Updated on October 21, 2024
About Our Contributors
Vincent Ayaga is a medical researcher and seasoned content writer with a bachelor's degree in Medical Microbiology. Specializing in disease investigation, prevention, and control, Vincent is dedicated to raising awareness about visual problems and the latest evidence-based solutions in ophthalmology. He strongly believes in the transformative power of ophthalmic education through research to inform and educate those seeking knowledge in eye health.
Dr. Melody Huang is an optometrist and freelance health writer with a passion for educating people about eye health. With her unique blend of clinical expertise and writing skills, Dr. Huang seeks to guide individuals towards healthier and happier lives. Her interests extend to Eastern medicine and integrative healthcare approaches. Outside of work, she enjoys exploring new skincare products, experimenting with food recipes, and spending time with her adopted cats.

